IVF vs IUI: Which Fertility Treatment Is Right for You?

Introduction
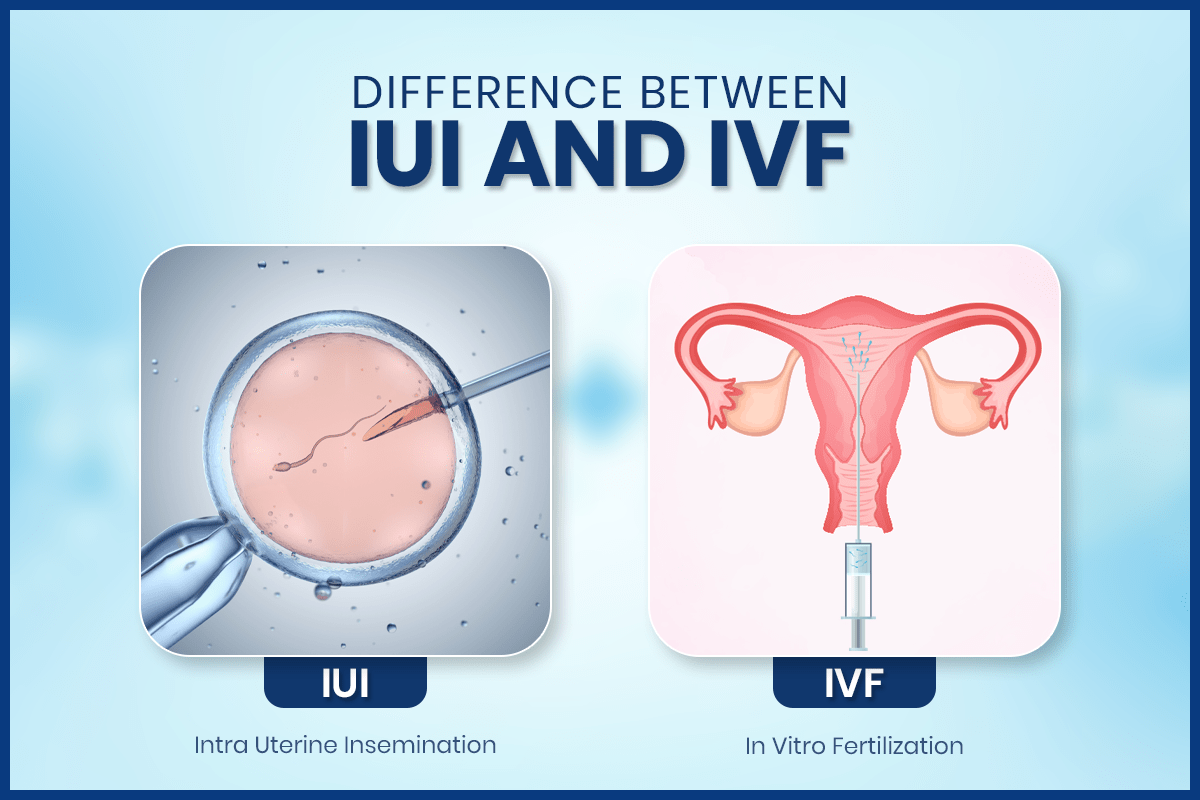
Choosing a fertility treatment can feel overwhelming, especially when you’re already navigating the emotional and physical challenges of trying to conceive. Two of the most commonly recommended options are IUI (Intrauterine Insemination) and IVF (In Vitro Fertilization). While both aim to help achieve pregnancy, they differ significantly in process, cost, success rates, and suitability.
Understanding how each treatment works—and who it’s best suited for—can help you make a more confident, informed decision alongside your fertility specialist.
Understanding the Basics of IUI and IVF
Before comparing the two, it’s important to understand what each treatment involves.
IUI is a less invasive fertility procedure where prepared sperm is placed directly into the uterus around the time of ovulation. The goal is to increase the chances of sperm reaching the egg naturally inside the body.
IVF, on the other hand, is a more advanced assisted reproductive technology. Eggs are retrieved from the ovaries, fertilized with sperm in a laboratory, and the resulting embryo is transferred into the uterus.
Both treatments are widely used, but they serve different fertility needs.
How IUI Works: A Simple Overview
IUI is often considered the first step in fertility treatment, especially for couples with mild fertility challenges.
The process typically includes monitoring ovulation, either naturally or with mild fertility medications. Around ovulation, sperm is washed and concentrated in a lab and then inserted directly into the uterus using a thin catheter. This short procedure is usually painless and completed within minutes.
IUI relies on natural fertilization occurring inside the body, which means at least one fallopian tube must be open and functional.
How IVF Works: A Step-by-Step Look
IVF is more complex but also more controlled.
The process begins with ovarian stimulation using hormone injections to encourage multiple eggs to mature. These eggs are then retrieved through a minor surgical procedure. In the lab, eggs are fertilized with sperm, and embryos are monitored for development. One or more healthy embryos are later transferred into the uterus.
Because fertilization happens outside the body, IVF bypasses several natural barriers, making it suitable for more complex fertility issues.
Success Rates: IVF vs IUI
Success rates are one of the most important factors for many couples.
IUI success rates are generally lower, averaging around 10–20% per cycle, depending on age, fertility diagnosis, and whether medications are used.
IVF success rates are significantly higher, often ranging from 40–60% per cycle for women under 35, with rates declining gradually with age.
For couples seeking the highest chance of success in a shorter time frame, IVF usually offers a clearer advantage.
Who Is IUI Best For?
IUI is commonly recommended for:
- Couples with unexplained infertility
- Mild male factor infertility (low sperm count or motility)
- Ovulation disorders that respond well to medication
- Cervical mucus issues
- Single women or same-sex couples using donor sperm
Because it is simpler and less invasive, IUI is often tried before moving to IVF.
Who Is IVF Best For?
IVF is typically recommended for more complex fertility challenges, such as:
- Blocked or damaged fallopian tubes
- Severe male factor infertility
- Endometriosis
- Low ovarian reserve or low AMH
- Failed IUI cycles
- Advanced maternal age
- Genetic conditions requiring embryo testing
IVF is also the preferred option when donor eggs, donor sperm, or gestational surrogacy are involved.
Cost Comparison: IVF vs IUI
Cost is often a deciding factor.
IUI is significantly more affordable, especially when done without medications. However, multiple cycles may be needed, which can increase overall expenses.
IVF is more expensive upfront, due to medications, lab procedures, and advanced technology. That said, its higher success rates can sometimes make it more cost-effective in the long run, especially for couples who would otherwise require many IUI cycles.
Physical and Emotional Considerations
IUI is generally easier on the body, involving fewer medications and minimal discomfort. Emotional stress may still be present, particularly if multiple cycles fail.
IVF requires injections, frequent monitoring, and invasive procedures, which can be physically demanding. Emotionally, IVF can be intense, but many patients also feel reassured by the level of control and precision involved.
Choosing the right treatment often depends on how prepared you feel—both physically and emotionally.
Risks and Side Effects
IUI risks are minimal but may include mild cramping, infection (rare), and an increased risk of twins if ovulation-inducing drugs are used.
IVF risks include ovarian hyperstimulation syndrome (OHSS), multiple pregnancy if more than one embryo is transferred, and emotional stress related to treatment outcomes.
A fertility specialist will tailor protocols to minimize risks in both treatments.
Time to Pregnancy: Which Is Faster?
IUI may take several cycles to succeed because it relies heavily on the body’s natural fertilization process. Even when ovulation is well-timed and sperm quality is adequate, there is still a degree of unpredictability. In cases of unexplained infertility or very mild fertility issues, doctors may not be addressing a clearly identifiable problem, which means each IUI cycle has a relatively modest chance of success. As a result, couples are often advised to try multiple cycles—sometimes three to six—before determining whether IUI is effective for them. While this stepwise approach is less invasive and more affordable initially, it can extend the overall time to pregnancy.
IVF, in contrast, often provides a faster and more direct path to pregnancy because several critical steps occur in a controlled laboratory setting. Fertilization does not depend on chance alone; eggs and sperm are carefully selected, combined, and monitored to ensure proper embryo development. Doctors can also choose the most viable embryos for transfer, which significantly improves the likelihood of implantation in each cycle. For couples who have been trying to conceive for several years, or for those facing age-related fertility decline where egg quality and quantity decrease over time, IVF can reduce the trial-and-error phase. By concentrating multiple chances into a single cycle, IVF may help save valuable time and offer clearer outcomes sooner.
IVF vs IUI: Key Differences at a Glance
While both treatments aim to achieve pregnancy, the key differences lie in complexity, success rates, and suitability. IUI is simpler, less invasive, and more affordable but has lower success rates. IVF is more involved and costly but offers higher success rates and greater flexibility for complex fertility needs.
How to Decide What’s Right for You
There’s no one-size-fits-all answer. The right choice depends on several factors, including:
- Age and ovarian reserve
- Fertility diagnosis
- Duration of infertility
- Budget and insurance coverage
- Emotional readiness
- Medical history
Many couples start with IUI and transition to IVF if needed, while others may benefit from going straight to IVF based on their circumstances.
Also Read: IVF After 35: Challenges, Advantages, and Success Strategies
Final Thoughts
Choosing between IVF and IUI is a deeply personal decision that should be guided by medical advice, realistic expectations, and emotional readiness. Both treatments have helped millions of people build families, and neither choice is “right” or “wrong”—only what’s right for you.
A consultation with a qualified fertility specialist can help clarify your options, set realistic goals, and create a treatment plan aligned with your body, your values, and your hopes for the future.
