Is IVF Painful? What Patients Can Realistically Expect
Introduction
One of the most common fears people have before starting IVF is pain. It’s a completely valid concern. IVF involves medical procedures, hormone injections, and emotional highs and lows—so it’s natural to wonder how uncomfortable the process really is.
The short truth is this: IVF is not pain-free, but it is usually far less painful than most people imagine. For many patients, IVF is more emotionally and mentally demanding than physically painful. Understanding what actually happens at each stage can significantly reduce anxiety and help you feel more prepared.
This guide walks through the IVF journey step by step, explaining what sensations patients typically experience, where discomfort may occur, and how clinics manage pain along the way.
Why IVF Is Often Perceived as Painful
IVF has a reputation for being painful largely because it involves needles, procedures, and hormone changes. For someone unfamiliar with medical treatments, that combination can sound intimidating. Online forums and second-hand stories sometimes amplify worst-case experiences, making IVF seem far more physically difficult than it usually is.
In reality, pain levels vary widely depending on individual tolerance, medical history, and emotional state. Most patients describe IVF as uncomfortable rather than painful, with brief moments of discomfort rather than ongoing pain.
Stage 1: Hormone Injections and Daily Shots
For many patients, injections are the first source of anxiety. IVF typically involves daily hormone injections for 8 to 12 days to stimulate the ovaries.
The needles used are very thin, similar to insulin needles. Most patients describe the sensation as a quick pinch or mild sting that lasts only a few seconds. After a few days, many people find the process becomes routine and far less intimidating.
Some soreness, bruising, or mild swelling at injection sites is common, especially if the same area is used repeatedly. Rotating injection sites and using proper technique helps minimize discomfort.
Emotionally, injections can feel more overwhelming than they are physically painful. Fear of needles, self-administration, and anticipation often contribute more stress than the injection itself.
Stage 2: Ovarian Stimulation Side Effects
As hormone levels rise, patients may experience physical sensations caused by ovarian stimulation rather than pain from procedures.
Common sensations include abdominal fullness, bloating, pressure in the lower abdomen, and mild cramping. These symptoms occur because the ovaries enlarge as multiple follicles develop. While this can feel uncomfortable, it is usually described as a heavy or tight feeling, not sharp pain.
Fatigue, mood swings, breast tenderness, and headaches are also common during this phase. These effects are linked to hormonal fluctuations rather than physical injury.
Most patients are still able to go about daily activities, though strenuous exercise is usually restricted to protect the ovaries.
Stage 3: Monitoring Appointments and Ultrasounds
During stimulation, frequent monitoring appointments are required. These typically involve blood tests and transvaginal ultrasounds.
Blood draws may cause brief discomfort similar to any routine blood test. Transvaginal ultrasounds can feel slightly uncomfortable, especially if the ovaries are enlarged, but they are generally not painful. The procedure is short and performed gently by experienced clinicians.
Patients who feel anxious or tense may perceive more discomfort, which is why relaxation and clear communication with the care team matter.
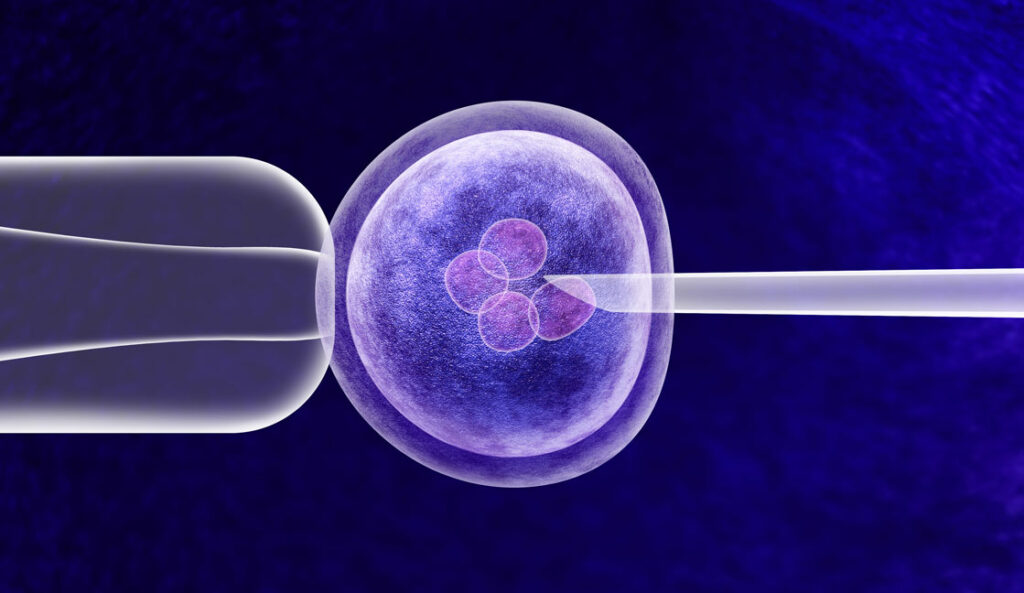
Stage 4: Egg Retrieval – Is This the Most Painful Part?
Egg retrieval is often the stage people fear most, but it is rarely painful during the procedure itself.
Egg retrieval is performed under sedation or light anesthesia. Patients are asleep or deeply relaxed and do not feel pain during the process. The procedure usually takes 15 to 30 minutes.
After waking up, some cramping, pressure, or soreness in the lower abdomen is normal. Many patients compare it to period cramps or post-ovulation discomfort. This discomfort typically lasts one to three days and is manageable with rest and mild pain relief recommended by the clinic.
Severe pain is uncommon and should always be reported to a healthcare provider.
Stage 5: Recovery After Egg Retrieval
The recovery period is where most physical discomfort occurs, but it is usually temporary.
Patients may experience bloating, abdominal tenderness, mild spotting, and fatigue. These symptoms gradually improve as hormone levels stabilize and the ovaries return to normal size.
Most patients return to light activities within a day or two. Full recovery usually happens within a week.
Clinics carefully monitor patients to reduce the risk of ovarian hyperstimulation syndrome (OHSS), a rare but more serious condition that can cause increased discomfort.
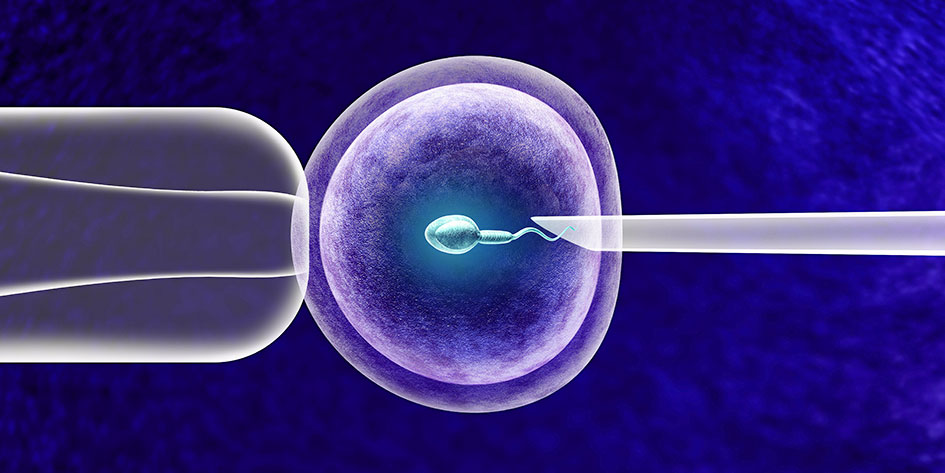
Stage 6: Embryo Transfer – What Does It Feel Like?
Embryo transfer is often described as the easiest and least uncomfortable part of IVF.
The procedure does not require anesthesia and is similar to a pap smear. Patients may feel slight pressure or mild cramping as the catheter is inserted, but it is generally quick and gentle.
Most people are surprised by how simple the transfer feels compared to what they expected. Afterward, some light cramping or spotting may occur, but many patients feel physically normal the same day.
The Two-Week Wait: Emotional vs Physical Sensations
After embryo transfer comes the two-week wait before pregnancy testing. Physically, most patients feel little to no pain during this phase.
Some may experience mild cramping, bloating, or breast tenderness, often caused by progesterone supplements rather than implantation itself. These symptoms can mimic early pregnancy signs, which can add emotional stress.
Emotionally, this stage can be the most challenging part of IVF. Anxiety, anticipation, and fear of disappointment often outweigh any physical discomfort.
Emotional Pain and IVF: An Important Reality
While IVF may not be intensely painful physically, the emotional strain can be significant. Uncertainty, hormonal changes, financial stress, and high expectations can all impact mental well-being.
Many patients describe emotional fatigue, mood swings, and moments of overwhelm. This emotional component is just as real as physical sensations and deserves attention and support.
Counseling, support groups, and open communication with partners and care teams can make a meaningful difference.
Does IVF Hurt More for Some People Than Others?
Yes, individual experiences vary.
People with conditions such as endometriosis, polycystic ovary syndrome, or pelvic sensitivity may experience more discomfort at certain stages. Pain tolerance, stress levels, and previous medical experiences also influence perception.
However, clinics personalize protocols and pain management strategies to reduce discomfort whenever possible.
How Clinics Manage Pain and Discomfort
Modern IVF clinics prioritize patient comfort. Sedation during egg retrieval, careful ultrasound techniques, and personalized medication protocols all help minimize pain.
Patients are encouraged to communicate openly about discomfort so adjustments can be made. Pain should never be dismissed or normalized without proper evaluation.
Tips to Reduce Discomfort During IVF
Staying hydrated, resting when needed, and following clinic instructions carefully can help reduce physical discomfort. Gentle movement, such as walking, may ease bloating, while avoiding intense exercise protects the ovaries.
Emotionally, having realistic expectations and a strong support system can significantly improve the experience. Understanding what is normal—and what is not—helps reduce fear.
So, Is IVF Painful Overall?
For most patients, IVF is not severely painful, but it is physically and emotionally demanding. The discomfort tends to be temporary, manageable, and closely monitored by medical professionals.
Many people who complete IVF say the process was less painful than expected, especially when compared to the anxiety they felt beforehand. The most challenging aspects are often emotional uncertainty and hormonal changes rather than physical pain.
Also Read: IVF After Miscarriage: When Is the Right Time to Try Again?
Final Thoughts
IVF is a medical journey that involves moments of discomfort, but it is designed to be as safe and tolerable as possible. Knowing what to expect transforms fear into preparedness.
Pain is not the defining feature of IVF. Instead, it is a process that requires patience, resilience, and support. For many patients, understanding the reality of IVF pain helps them approach treatment with confidence rather than fear.
If you’re considering IVF, asking questions, preparing mentally, and choosing a supportive care team can make the experience far more manageable—both physically and emotionally.
